Boston, October 27, 2020 –Consumer digital bill payment trends have increased over the past four years across payment channels, payment methods, payment frequency, and bill delivery methods. This propensity to transact and engage digitally within the bill presentment and payment process occurs as household-level trends increase in parallel. As these trends take hold, it is increasingly important for health plans and their payments partners to operate across a four-pronged approach that considers channels, methods, frequency, and bill delivery.
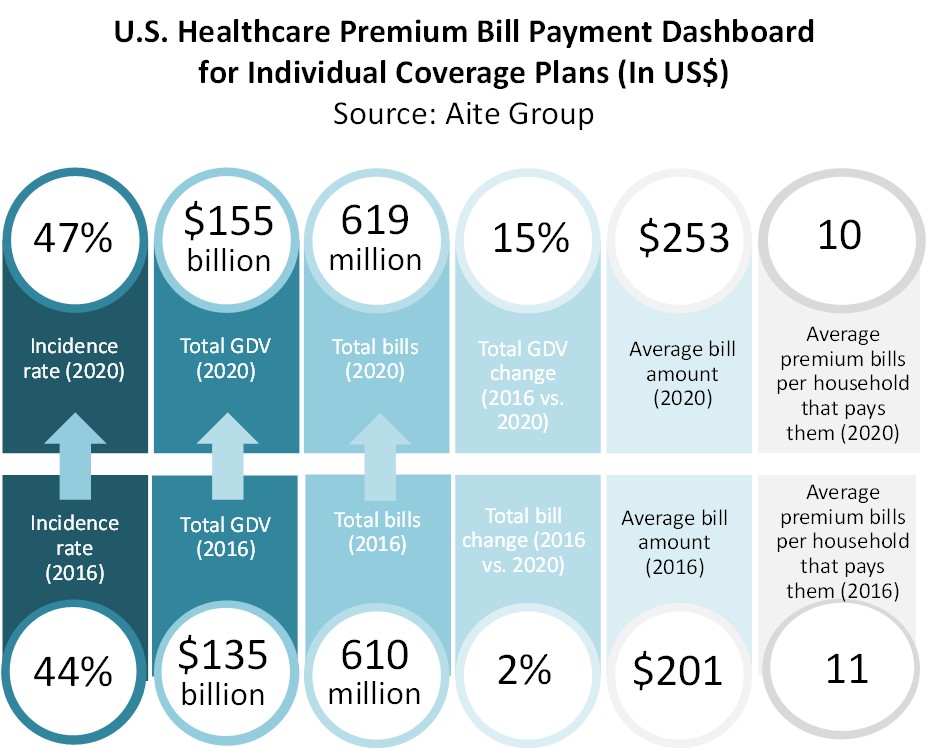
This report compares the market size and key trends from 2016 to 2020 sizing channels, methods, frequencies, and bill delivery methods, and it offers insights into the minds of the consumers, developing a profile of their ability and wherewithal to pay bills. It is based on a Q2 2020 Aite Group survey of 3,039 U.S. consumers, in which 1,428 consumers indicated their household paid a bill for an individual coverage plan premium between March 2019 and March 2020.
This 40-page Impact Report contains 37 figures and five tables. Clients of Aite Group’s Health Insurance service can download this report, the corresponding charts, and the Executive Impact Deck.
This report mentions PayPal.
About the Author
Datos Insights
We are the advisor of choice to the banking, insurance, securities, and retail technology industries–both the financial institutions and the technology providers who serve them. The Datos Insights mission is to help our clients make better technology decisions so they can protect and grow their customers’ assets.