Boston, April 14, 2021 – Artificial intelligence offers a bounty of benefits, but the healthcare industry is not often clear on how to capitalize on those benefits. Vendors have been hard at work fine-tuning and sharpening their AI and robotic process automation capabilities to ensure their products and solutions align with the needs of health systems and health plans. What are the use cases in healthcare payments that stand to benefit from these tools?
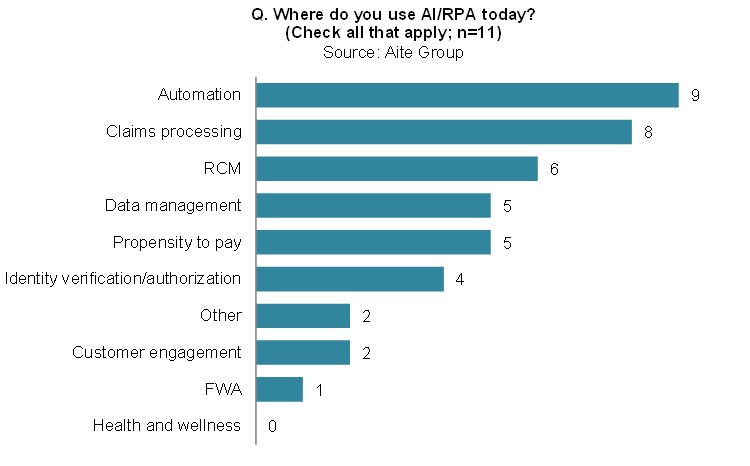
This report outlines 10 use cases that harness AI in the health insurance segment and identifies which ones resonate strongly with providers and their revenue cycle managers. To form the basis of this report, Aite Group interviewed 30 executives distributed across health systems’ finance and revenue cycle executives, health plan executives, and vendors with AI/RPA capabilities with a presence in healthcare payments. These interviews were conducted throughout Q1 2020 with additional secondary research on developments from Q2 2020 to Q1 2021.
This 27-page Impact Report contains seven figures and one table. Clients of Aite Group’s Health Insurance service can download this report, the corresponding charts, and the Executive Impact Deck.
This report mentions Accolade, Acuant, Aetna (acquired by CVS Health), Appian, Apple Health, Arise, Auth0 (in the process of being acquired by Okta), Buoy Health, Cedar, Cerner, CGI Technologies, Change Healthcare, Chisel AI, ClarisHealth, Codoxo, CogniCor, Conifer Health, Cotiviti, Elavon, Engati, EPIC, Experian, Fitbit, Garmin, GoodRx, Harland Clarke, HealthcareFraudShield, HMS (currently in the process of being acquired by Gainwell), ID Assist, ID.me, IDology, Infinx, Infutor, InstaMed (acquired by JPMorgan), Intel, Integrity Advantage, iVita Financial, Jawbone, Jumio, Kareo, nThrive, LexisNexis Risk Solutions (ThreatMetrix), Mastercard, Mitek Systems, Olive AI, Optum Financial/OptumInsight, Meditech, NuData (a Mastercard company), Okta, PatientPay, PingIO, RSA, SailPoint, SAS Institute, Shift Technology, Socure, Sonic Boom Wellness, Simplee (acquired by Flywire), SwervePay, TransUnion, Trulioo, Twilio, Veratad, VisiQuate, VisitPay, Vitality, Weight Watchers, Wellable, Wellsource, Welltok, UiPath, WDG Automation (acquired by IBM), Wind River Financial, Xtend Healthcare, and Zendesk.
About the Author
Datos Insights
We are the advisor of choice to the banking, insurance, securities, and retail technology industries–both the financial institutions and the technology providers who serve them. The Datos Insights mission is to help our clients make better technology decisions so they can protect and grow their customers’ assets.