Boston, May 4, 2021 – A consolidating competitive landscape, a slew of regulatory shifts and changes, and a raft of technology advances offer payment integrity vendors both opportunities and challenges in the healthcare space. A range of other factors—from integrating acquisitions into one cohesive product offering, the increasing need for robust data, the aim to reduce provider abrasion, an emphasis on increasing the level of payment accuracy, and the attention on emerging business and reimbursement models—will constitute the road signs on the path ahead for payment integrity.
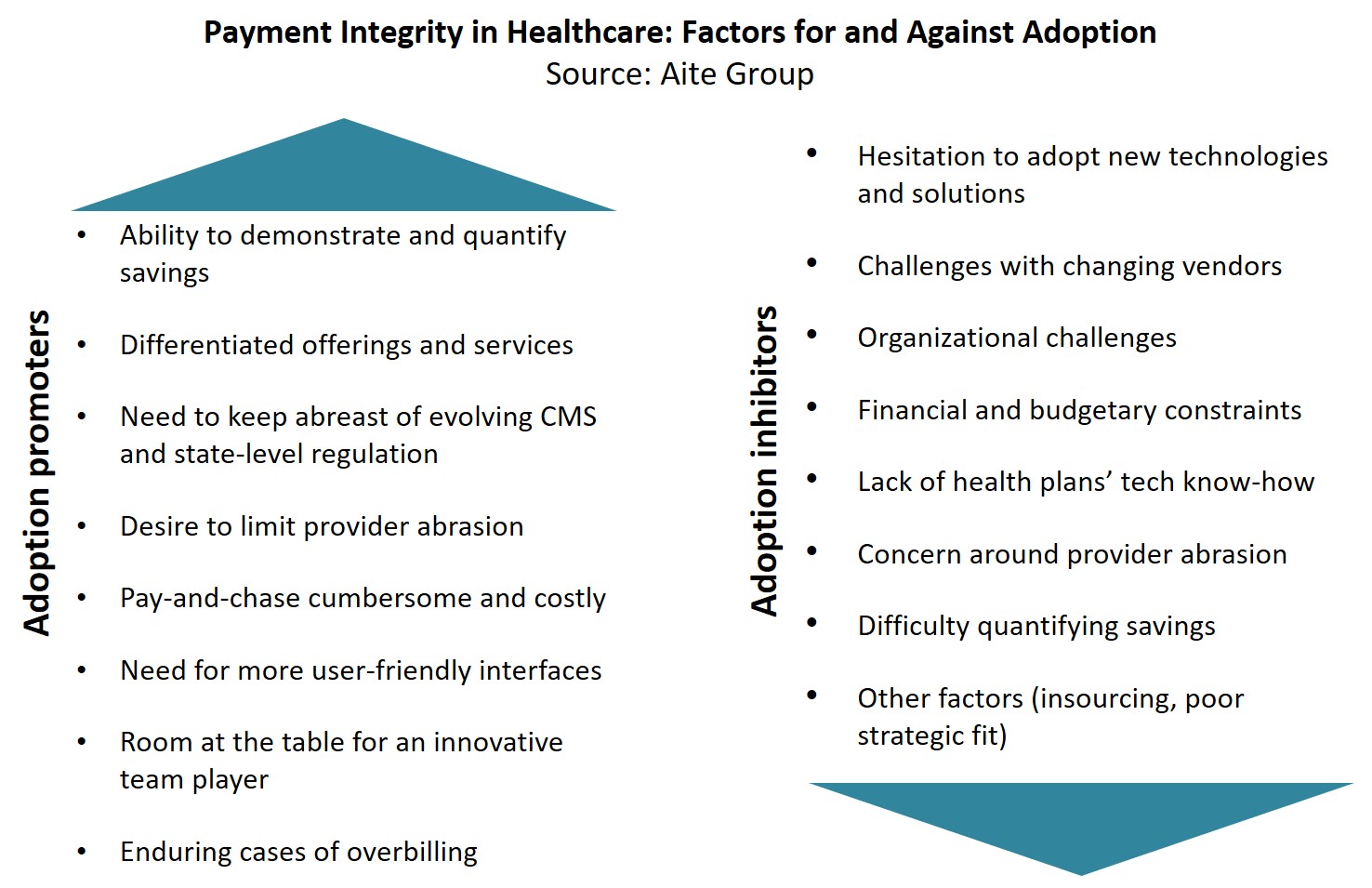
This report evaluates the payment integrity market, lists key market trends affecting payment integrity specific to healthcare claims, and sizes the market using multiple metrics. The report also discusses the drivers that fuel as well as hinder adoption of payment integrity and payment accuracy solutions. It is based on discussions with leading vendors as well as active end clients and other key players participating in this technology market ecosystem; a forthcoming Aite Matrix report will provide a formal evaluation of leading payment integrity vendors through Aite Group’s proprietary vendor assessment framework.
This 29-page Impact Report contains 12 figures and two tables. Clients of Aite Group’s Health Insurance service can download this report, the corresponding charts, and the Executive Impact Deck.
This report mentions Centers for Medicare and Medicaid Services, CGI Group, Equian (acquired by Optum), Change Healthcare (acquired by Optum), ClaimLogiq, ClarisHealth, Codoxo, Cotiviti (acquired by Veritas Capital Fund Management), Discovery Health Partners, EXL Service, Experian Health, Healthcare Fraud Shield, HMS (acquired by Gainwell), IBM Health, Integrity Advantage, LexisNexis Risk Solutions, Mastercard Health Solutions, Multiplan, Optum Financial, Qlarant, Performant, SAS Institute, SCIO Analytics (acquired by EXL Service), Shift Technologies, Truven Health (acquired by IBM), and Zelis.
About the Author
Datos Insights
We are the advisor of choice to the banking, insurance, securities, and retail technology industries–both the financial institutions and the technology providers who serve them. The Datos Insights mission is to help our clients make better technology decisions so they can protect and grow their customers’ assets.